Optimizing Antibiotic Stewardship in California NICUs
March 2021 – February 2023
 The Optimizing Antibiotic Stewardship in California NICUs (OASCN) Collaborative aimed to scale up dissemination of various nationally recommended interventions to improve antimicrobial stewardship among NICUs in California using a blended QI collaborative and ECHO™ (Extension for Community Healthcare Outcomes) tele-learning model. ECHO™ is an evidence-based, American Academy of Pediatrics-endorsed method of practice dissemination used globally that focuses on faculty-facilitated, case-based learning tailored to how clinicians are inclined to learn and build practice consensus. QI collaboratives, while similarly including faculty facilitation and peer-learning, focus on supporting continuous quality improvement efforts by site implementation teams. OASCN was supported by a grant from the Agency for Healthcare Research and Quality (AHRQ Grant# R18HS26168-01A1) to implement and evaluate the collaborative.
The Optimizing Antibiotic Stewardship in California NICUs (OASCN) Collaborative aimed to scale up dissemination of various nationally recommended interventions to improve antimicrobial stewardship among NICUs in California using a blended QI collaborative and ECHO™ (Extension for Community Healthcare Outcomes) tele-learning model. ECHO™ is an evidence-based, American Academy of Pediatrics-endorsed method of practice dissemination used globally that focuses on faculty-facilitated, case-based learning tailored to how clinicians are inclined to learn and build practice consensus. QI collaboratives, while similarly including faculty facilitation and peer-learning, focus on supporting continuous quality improvement efforts by site implementation teams. OASCN was supported by a grant from the Agency for Healthcare Research and Quality (AHRQ Grant# R18HS26168-01A1) to implement and evaluate the collaborative.
OASCN began with 31 California NICUs and hosted Learning Sessions open to all NICU clinical staff via Zoom every 2 weeks from early March 2021 through February 2022 and quarterly thereafter until February 2023. Other collaborative activities and supports included a Learning Points recap email after each biweekly session, a collaborative email listserv and filesharing site, and an online data submission and QI analytics portal. The primary goal of the OASCN Collaborative was to safely reduce antibiotic usage rate (AUR) for all infants at participating NICUs. Participating NICUs selected which gestational ages to focus their improvement efforts (e.g. preterm, late preterm, term babies). An OASCN Resource Bundle can be found on the OASCN Resource Bundle page and includes resources by topic areas as well as standalone documents that compile all the OASCN Learning Points and NICU Stewardship literature references.
Related Publication: Blood culture procedures and practices in the neonatal intensive care unit: A survey of a large multicenter collaborative in California
Mother and Baby Substance Exposure Initiative
January 2019 - September 2020
 The Mother & Baby Substance Exposure Initiative (MBSEI) was a joint partnership between CPQCC, the California Maternal Quality Care Collaborative (CMQCC), and Health Management Associates (HMA) to improve outcomes for mothers and newborns impacted by substance exposure, with a specific focus on Opioid Use Disorder.
The Mother & Baby Substance Exposure Initiative (MBSEI) was a joint partnership between CPQCC, the California Maternal Quality Care Collaborative (CMQCC), and Health Management Associates (HMA) to improve outcomes for mothers and newborns impacted by substance exposure, with a specific focus on Opioid Use Disorder.
MBSEI emphasized care that maintains the mother-baby dyad throughout the hospital stay and addresses treatment and prevention of substance exposure both during and after pregnancy. The initiative included a statewide collaborative involving obstetric and neonatal teams at 37 hospitals and the development of an interactive online toolkit on perinatal substance exposure for maternal and newborn care providers. The Mother & Baby Substance Exposure Initiative was funded by the California Department of Health Care Services (DHCS) as part of a Substance Abuse and Mental Health Services Administration (SAMHSA) State Opioid Response grant. While this project has formally ended, the Maternal Substance Exposure Initiative (MatEx) Database is still collecting data and actively recruiting centers interested in improving care for infants with substance exposure.
In Situ Simulation
April 2018 – April 2020
CPQCC's Simulating Success Collaborative was designed to help NICUs implement simulation-based neonatal resuscitation training programs at their hospitals to improve resuscitation team performance during preterm and term deliveries. Simulation-based learning can improve the safety, efficiency, and effectiveness of neonatal resuscitation. Safe, effective, and efficient resuscitation team performance can help prevent neonatal mortality and serious morbidities such as bronchopulmonary dysplasia (BPD) and hypoxic-ischemic encephalopathy (HIE).14 NICU teams participated in the collaborative. The teams were divided into four groups, each of which completed a 15-month program, which included three months of preparatory training followed by 12 months of running simulation and debrief sessions. CPQCC is grateful for its partnership with the Stanford Center for Pediatric & Perinatal Education (CAPE) in implementing the Simulating Success Collaborative and the extensive expertise in simulation that they brought to the initiative.
Antibiotic Stewardship
June 2016 to November 2017
CPQCC's Antibiotic Stewardship Collaborative included 28 of our member NICUs, the largest group to date, and aimed to reduce antibiotic utilization rates through the application of a bundle of best practices, including routine antibiotic “time-outs” 48-72 hours after obtaining cultures. Preliminary findings indicate that the collaborative group eliminated roughly 11,700 “antibiotic days” across California and safely decreased the antibiotic utilization rate (AUR) by 13.8%. These improvements helped to decrease the risk of antibiotic resistance and adverse drug events as well as the cost of care at these NICUs.
 Optimizing Length of Separation
Optimizing Length of Separation
June 2013 to May 2015
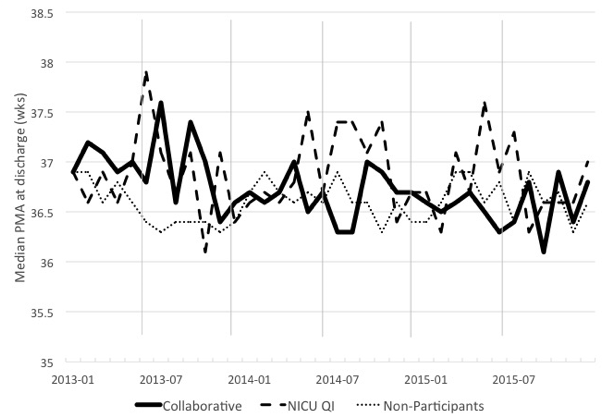
20 of our member NICUs participated in the Optimizing Length of Separation Collaborative, which aimed to reduce the length of hospital stay by three days for infants born between 27-32 weeks gestational age. Participants were encouraged to use a standardized approach to feeding, discharge planning, and apnea/bradycardia management in order to achieve this aim. By the end of the 18-month collaborative, participants decreased length of separation by three days and increased early discharge (before 36 weeks, 5 days) to 41.9% from 31.6%.
Related Publication: Comparison of Collaborative Versus Single-Site Improvement to Reduce NICU Length of Stay
Delivery Room Management 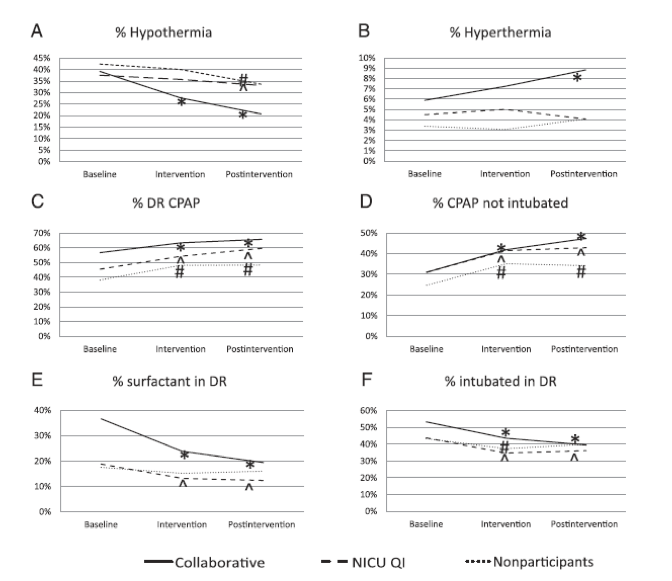
June 2011 to November 2012
The 20 hospitals in the Delivery Room Management Collaborative saw a collective decrease in hypothermia, delivery room intubation, and surfactant administration as a result of their participation. The project aimed to improve management of high-risk deliveries through the implementation of a best practice bundle that included strategies to avoid hypothermia; establish lung volume in the least-invasive manner; and support teamwork with checklists, briefings, and debriefings.
Related publication: Implementation methods for delivery room management: a quality improvement comparison study
 Breastmilk Nutrition
Breastmilk Nutrition
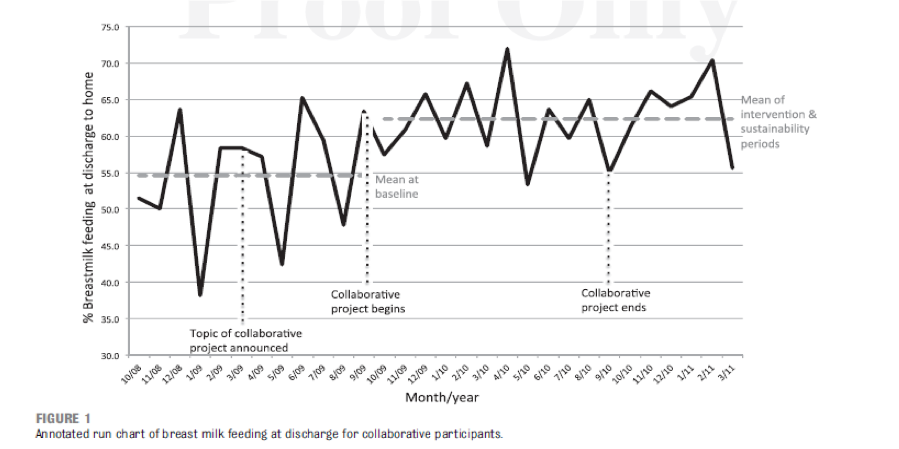
September 2009 to April 2011
11 CPQCC NICUs participated in a collaborative designed to increase breastmilk feeding rates for VLBW infants through implementation of a set of best practices outlined in the CPQCC Nutritional Support of the VLBW Infant Toolkit. The toolkit was subsequently updated in 2018. By the end of the collaborative, participants had increased breastmilk feeding at discharge to 64%, from 54.6% at the start of the collaborative. Participants also saw a decrease in NEC rates from 7% to 2.4%.
Related publication: Perspectives on Promoting Breastmilk Feedings for Premature Infants During a Quality Improvement Project
Healthcare-Associated Infections
February 2008 to January 2009
The 19 NICUs in the Healthcare Associated Infections Collaborative decreased catheter-associated bloodstream infections (CABSIs) by 75% in infants with birth weights ≤ 1500 grams. The project aimed to reduce the occurrence of CABSI to almost zero system-wide.

